Book An Appointment Via Whatsapp
(21) 97136-0040
(21) 97136-0040
Definition
The term osteoarthritis (OA) denotes a progressive and degenerative wear-and-tear of the joint. It usually occurs most often in people 50 years of age and older. However, other conditions can accelerate this process. Trauma, poorly managed joint fractures, infection, chronic mechanical overload (physical activity routine without correct monitoring) are some examples. The tissue lining the joints is called cartilage. A white film that does not regenerate and, as it deteriorates, exposes the most superficial layer of the bones. Patients begin to feel great pain, angular deformity, and loss of movement.
It’s a serious orthopedic problem. It causes a lot of suffering to the patient, who loses his normal movement, lives with a lot of pain and in many cases starts to depend on others to leave the house and carry out daily activities.
Which are the most commonly affected joints by this orthopedic disease?
OA can affect any joint in the body. However, we observe in our practice more symptoms in the hips, knees, and lumbar spine. These are the sites most exposed to trauma and that receive the biggest mechanical load on a daily basis. Naturally, these are the places most prone to degeneration and pain.
In most cases, those affected initiate a treatment on their own. In the early stages of the disease, they experience only low intensity pain and, at first, do not seek a specialist. Often this self-treatment is inadequate as the disease progresses and the pain increases. Finally, when they do see a doctor, the disease is much more advanced and difficult to recover from.
How is osteoarthritis diagnosed?
We always start by listening to the patient. Medical history is very important and guides us through the diagnostic possibilities. A calm assessment and time to listen to the patient are critical in this process. We orthopedists have an arsenal of physical tests that helps us to deepen our reasoning and arrive at a very consistent diagnostic hypothesis in the first consultation. We can often resort to imaging exams. It is important to emphasize that requesting the correct exam is essential for the evaluation. Most of the time, a common X-ray is enough for the diagnosis, but in some cases we can ask for an MRI and CT scan to confirm the diagnosis.
What are the treatment options for osteoarthritis?
There is no fixed protocol. Patients receive a tailored treatment plan based on their medical history and the stage of the disease. We have many resources that, when used correctly, improve pain, range of motion and the patient’s quality of life.
Physical Therapy
Physical therapy has evolved a lot in recent years. Strengthening of specific muscle groups, myofascial release reducing tension in the myofascial chain and manual therapy techniques are what we use in most cases. Postural re-education and specific resources for pain control are also important and can be used in patients with specific needs.
In my team, I work with specialized physical therapists with extensive experience in treating patients with OA. When well indicated and conducted, physical therapy is essential for recovery.
Biologics
Biologics are a subset of medications. Chondroprotective agents are a type of biologic drug that inhibits the inflammatory chain that degrades cartilage. They act by preserving viable tissue and in the medium and long term ensure a healthier joint. These are drugs used for longer periods of time and, even though they act on inflammatory cytokines, they do not harm, in general, the stomach and the kidneys. Obviously, all medication must be prescribed after medical evaluation and self-medication is always dangerous.


Surgical Options
These surgeries are indicated for younger patients in whom we do not want to perform an arthroplasty. Its fundamental concept is simple, but the surgery is also invasive and has specific needs and specialized rehabilitation in the postoperative period. It consists of cutting the bone to change the angle of the joint. By doing so, we remove the load from the affected area of the joint and “shift” it to another still healthy area with a large amount of cartilage. It is a procedure that greatly improves pain and extends the useful life of the joint. The cutting angles are measured on the computer and a three-dimensional model in our test bone, called a “template”, is made. The surgical planning in this case is essential for the desired successful outcome.
Also called partial replacement surgery, in this procedure only one side of the joint is replaced with implants (prostheses). That is, we replace only the injured compartment of the knee, preserving the healthy part and maintaining its bone and cartilaginous stock. It is a more conservative surgery, but we have very strict criteria for indicating the technique.
In this surgery, also known as total replacement surgery, the entire joint is replaced. These are curative surgeries, with a high degree of patient satisfaction when well indicated and performed. The entire affected area of the joint is replaced by a modern implant, usually in a cobalt chromium alloy and polyethylene or ceramic. All components are measured to ensure replacement within the most anatomical parameters. My team is multidisciplinary. We do a judicious surgical risk preparing the patient for the surgery with the most modern resources. The pre and postoperative physical therapy protocol is performed daily by trained and specialized physical therapists on the team. The clinicians monitor the hospitalized patient on a daily basis, ensuring a quick and safe recovery.
Viscosupplementation is a procedure in which hyaluronic acid is injected into the joint. As the application is local, its effects tend to be more expressive and lasting. Its function is also to protect and improve the biological condition of the cartilage and to lubricate the dynamics of movement. The procedure must be done very responsibly. Specific products to carry out asepsis are used, and the site of injection must respect the local anatomy without harming nerves, muscles or tendons. In some cases, we can use an ultrasound. This device shows the exact location where we should position the needle. Through a video screen and a transducer, we are able to see the structures and the easiest and safest place to perform the procedure.
There are several products with different compositions and molecular weight. The correct way to carry out the procedure, the product most suited to the patient’s profile, and the frequency of treatment is individually recommended on a case-by-case basis. With the correct indication, the results are excellent, and patients feel the benefits in the first months after the injection.
When a bone breaks, a series of local and systemic consequences unfolds. Different from what most think, breaking a bone is a serious event, which can ensue a series of complications. It’s not just the bone tissue that suffers, but all the others as well.
A femur fracture in an elderly patient, for example, can precipitate cardiac overload, paralyze the intestine, lead to skin wounds (the patient is unable to move, causing pressure ulcers), cause vein thrombosis, among other things. These are extremely challenging injuries for the surgeon (no fracture is the same) and the physician must have great skill and a specialized team in order to minimize risks and ensure patients recover as soon as possible.
Sometimes fractures in young adults can be more difficult to resolve. These patients have more vitality, strength, and bone quality. In general, fractures in young adults are a result of severe trauma and can cause fragmentation of the joint and produce combined injuries that are harder to treat. Besides, people of this group are at their peak of productivity. An inadequate solution or permanent sequela can mean a very large financial and social impact. The approach to fractures in both elderly and younger patients is complex, requires a lot of responsibility and can have a disastrous impact if mishandled.
What are the main complications of fractures in elderly patients?
Confinement to bed and other mobility restrictions imposed by the fracture can generate a series of complications. The most common fractures are those that affect the femur, but in other parts of the body they can also be very serious with equally worrying repercussions. Here are some of the most frequent complications in these cases:
Is treatment always surgical?
No. There are well-defined criteria for recommending surgery. Most fractures can be managed conservatively, with clinical follow-up and rehabilitation. It should be noted that non-surgical treatment is also complex, it depends on the patient’s engagement in following medical guidelines. In general, it takes longer to recover and needs adequate immobilization.
Hands have a complex system of tendons and pulleys that works harmoniously to create movement in the fingers. This complex system makes it possible to interact with the world and carry out daily activities. Hands are used to type, use a mouse, open doors, grab glasses and bottles, etc. It is the primary site of the body in terms of day-to-day function and use.
Over time, these pulleys can become rigid and less compliant, hindering the sliding of the tendon inside. The increased friction between these two tissues ends up generating inadequate movement of the affected digit and may even “lock” it in a bent position. This can be very uncomfortable, and, in the most severe cases, patients may remain for long periods with the finger locked in flexion. This condition is most common in patients over the age of 50 and the most frequently affected pulley is the A2 located between the beginning of the fingers and the palm of the hand.
What are the most common forms of trigger finger and how to treat it?
Trigger finger does not have a specific classification. Generally, diagnosis is made after an orthopedic evaluation and the severity of the condition is determined by finger mobility, frequency, and intensity of locking. Once the disease and its stage are identified, we can treat it with the most appropriate resources. There is a variety of treatment options including:
Physical therapy
A physical therapist, through a number of manual treatments, will try to improve tendon-pulley interaction, reducing friction and helping regain movement. Several techniques can compose the treatment and, in many cases, satisfactory results are observed. We usually prescribe rehabilitation for patients in the early and moderate stages of the condition. These are the ones with the best results. Some of the outstanding physical therapy procedures for these cases are:
It is important to emphasize that there is no fixed protocol. Each patient receives a tailored treatment according to their individual physiology, injury severity, social aspects, age range and level of functional independence.
Injections
Liquid anti-inflammatory substances can be injected inside a joint or functional unit/complex. In moderate cases of trigger finger, it is a very accepted resource and can produce satisfactory results in many cases. This is an in-office procedure with local anesthesia and total safety. We follow a strict standard of asepsis and antisepsis. The injection reduces local edema and decreases the pressure inside the pulley, improving the tendon-pulley interaction. An improvement in the movement of the digit and, consequently, in the clinical condition of the patient is expected.
Surgery
Surgical procedure is reserved for severe cases or for those that did not improve with conservative treatment. We open the pulley, freeing the tendon to move and make the finger flexion movement. It is a day surgery procedure (the patient stays in the hospital for a maximum of 8 hours), performed under local anesthesia and relief is usually almost immediate. In the vast majority of cases, the treatment is so effective that physical therapy is not necessary, and the condition is completely healed in 2 to 3 weeks. Surgery is performed through a small open incision that is closed with an aesthetic suture that after a few months becomes almost imperceptible.

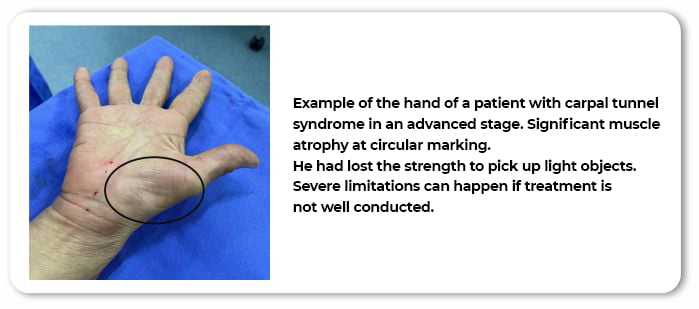
Carpal tunnel syndrome or median nerve compression syndrome is a very common condition that usually occurs in women over 45 years of age. Currently, there is research on why this is the case, with researchers looking at the hormonal changes women in this age group deal with. What we know for sure is that it is a hardening of a wrist tissue called the flexor retinaculum, causing nerve compression. The compressed nerve swells and causes the symptoms. Patients report a lot of tingling in the palm of the hand, may feel temperature changes and, in more advanced stages, may lose strength and start dropping objects (such as cups and plates).
How do you know a patient has symptoms?
Medical history is very suggestive. There are specific physical tests performed to diagnose the condition, most of the time the diagnosis is formulated at the first consultation. Complementary exams can be used to help confirm the diagnosis in cases of doubt or to help define the severity of the condition.
Why is numbness the most common symptom?
In orthopedics “numbness” is called paresthesia. Paresthesia is a change in sensitivity, a classic symptom of peripheral neurological injury. It can manifest itself in the entire territory where the peripheral nerve acts (dermatome). Testing sensitivity in the index fingertip is crucial in defining that it is a median nerve injury (carpal tunnel syndrome). There are several other neurological syndromes that can affect the hand and reaching the correct diagnosis is very important. For instance, a herniated disk in the cervical spine can give very similar symptoms.
What is the treatment?
There are several treatment options. The clinical aspects as well as the stage of the condition must be considered when choosing the most suitable one.
Physical therapy
In early stages, specific techniques such as myofascial release therapy, instrumental fibrolysis (hooks), stretching, and physical exercises that can produce satisfactory results.
Injections and oral medication
Anti-inflammatory medications can be injected into the carpal tunnel, helping reduce swelling and relieve painful symptoms. Injections must be performed with great care and by skilled professionals. When performed incorrectly, they can worsen the condition. We emphasize that this is an adjunctive therapy that must be performed within a broader context of treatment. Isolated it is a palliative measure and its positive effects may be temporary.
Treatment options also include oral medication. There are different drugs that can help control symptoms and reverse the condition. We always recommend the best path following strict medical criteria and each patient must get an individualized treatment.
Surgery
Surgery consists of opening the flexor retinaculum of the wrist. It is a percutaneous procedure performed under local anesthesia by making a small1-inch incision in the palm, and patients remain in the hospital for a few hours. By opening the retinaculum, pressure on the nerve decreases and immediately improves the neurological flow, allowing the tissue to heal. It is important to highlight some very important aspects:
The suffix “ITIS” means inflammation. A painful process that is characterized by 5 fundamental points: heat, redness of the inflamed, pain, edema or local swelling, and loss of function with difficulty in performing daily tasks. When this inflammatory process occurs in the elbow, we call it epicondylitis, which can be lateral or medial. Epicondylitis is also known as “tennis elbow” (lateral) and “golfer’s elbow” (medial).
There may be several causes for the condition, but what we most commonly observe are injuries caused by repetitive effort. The overload of the wrist musculature leads to stress on the musculotendinous complex, causing tissue inflammation and sometimes even tears.
What are the symptoms? What do patients feel?
Symptoms can start insidiously, that is, with a minor, non-disabling pain. This “discomfort” gets worse over time until, at a certain point, the pain starts to limit the patient’s motility. Small tasks start to get difficult: typing on the computer, picking up objects and even putting your hair up can become a challenge. Elbow palpation can be extremely painful, and the area can be very tender. For high-performance athletes, it can often impair performance in the game and disrupt professional life.
What are the treatment options?
Injection
In the most acute periods, anti-inflammatory medication can be injected into the tendon and around it. Local application promotes rapid relief of symptoms and may aid rehabilitation. It must be done aseptically and there is a fixed protocol and appropriate drugs for this procedure. It is performed in-office and with local anesthesia.
Cryotherapy
Especially in the inflammatory phase, ice packs applied locally are an important tool for relieving and improving pain. Ice promotes a reduction in temperature and consequently a reduction in local vascularization, thus decreasing the pain and helping improve some aspects of inflammation.
Physical therapy
Physical therapy offers a series of specific techniques to improve local muscle dynamics and release tension and fibrosis. The so-called manual therapy is very important for recovery in these cases. Stretching and strengthening techniques are part of a comprehensive treatment and are used according to the moment and stage of the condition, as well as to the patient’s individual needs. There is no fixed protocol.
Epicondylitis can manifest itself in different stages and the patient can evolve in different ways during treatment, presenting specific needs that the physical therapist must detect and implement changes accordingly. Treatment must always be individualized.
Shockwave therapy
A relatively new technique that has shown promising results in cases of subacute and chronic epicondylitis (those that are taking a long time to improve despite treatment and rehabilitation). Through a transducer and a shockwave device, the doctor sends shockwaves into the injured areas. Potency and number of sessions must be determined on a case-by-case basis.
Surgery
Surgical treatment is the exception for this injury. However, if nonsurgical treatments fail and the disabling and painful symptoms persist, surgery becomes an alternative with excellent outcomes. It is performed arthroscopically under brachial plexus block (a very mild anesthesia and with low incidence of side effects), and the scar left is very small. Generally, the patient remains hospitalized for a maximum of 12 to 24 hours. It requires specific physical rehabilitation and patients most often return to their daily activities within weeks.
Dr. Daniel Ramallo dreamed of becoming a doctor since childhood. A dream that required dedication, abdication, and effort. He devoted himself to his studies to best serve his patients with state-of-the-art care in a highly personal, comprehensive and compassionate manner.