Book An Appointment Via Whatsapp
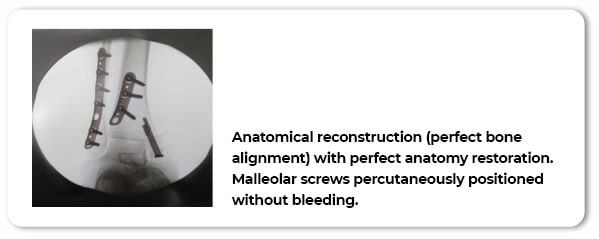
(21) 97136-0040
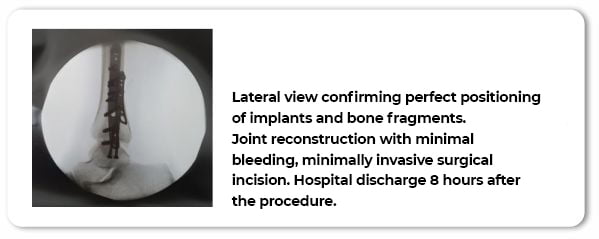
(21) 97136-0040
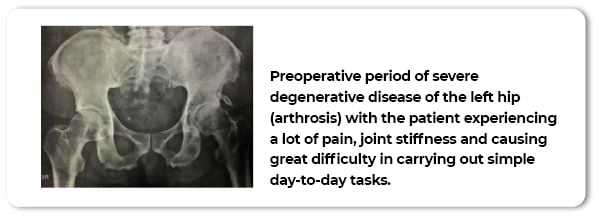
Over the course of the years, joints that carry the weight of the body (load joints) suffer a natural wear and tear that can lead to a lot of pain. There are many treatment options that help preserve the joint when used correctly and at the early stages, but in more advanced cases replacing the hip with prosthetic components is the only solution.
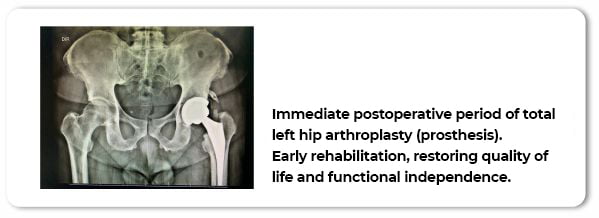
Hip replacement, also known as hip arthroplasty, is a surgical procedure that replaces the damaged hip with a new artificial one. This technique has evolved a lot in recent years. Our approach is what we call minimally invasive, with a smaller incision to access the hip which results in a minimized impact of surgery on healthy tissues. On the day after the surgical procedure, patients begin physical rehabilitation: standing up, putting weight on the joint and gait practicing with a physical therapist. Pain relief and mobility gain is significant, making this a technique with the highest patient satisfaction rate.
Hip replacement surgery can be performed using different ways to access the hip depending on the individual needs of the patient. Additionally, choosing the best implant (prosthesis) depends on the patient’s physical characteristics and the surgeon’s experience. A surgeon with extensive experience in hip arthroplasty is essential in the process, making all the difference in the final surgical result.
How is the surgery done?
As previously stated, each patient is unique: body composition and needs may vary from case to case. In general, there are four different surgical approaches, and each has an advantage; we use the one that is most suited for the patient. At our practice, we always use minimally invasive methods. We use positioners and specific instruments that allow for a minor impact and therefore a faster, safer surgery that preserves the musculature and adjacent tissues. Some patients want a very aesthetic suture and for that we have a renowned plastic surgery team performing dermal suture with stellar outcomes.
Recovery after surgery
We work with early rehabilitation; physical stimulation begins 6 hours after surgery. Our team of physical therapists works to improve blood flow, reduce swelling, correct posture and breathing in the first hours after the procedure. We do not work with fixed protocols and rehabilitation is adjusted to each patient’s profile with an individualized and comprehensive approach. In most cases, patients are discharged walking (with assistance) and putting full weight on the operated hip without feeling pain.
Joints have a protective tissue called articular cartilage. This cartilage wears away over the years leading to bone exposure and pain. This type of injury is increasingly more common in adult patients. It also affects professional and amateur athletes due to an overuse of the joints from physical activity, causing a lot of pain, discomfort, and loss of function. The most affected joint is the knee, but we also observe this condition in the hip and the shoulder.
Patients have a number of treatment options in this case. The goal is to preserve the joint and avoid the need for surgical intervention (arthroplasty). A very consolidated therapy with excellent results is the injection of hyaluronic acid into the joint. This product, when used with the correct indication, improves joint lubrication, promotes cartilage nutrition and improves the local biological environment, ensuring symptom relief and return to sports activities without surgery.
Comprehensive treatment is complex and requires medical follow-up for excellent results. An experienced and specialized orthopedist is essential for a successful outcome. Come get a medical evaluation.
How is it done?
The procedure is performed on an outpatient basis under local anesthesia. In some cases, imaging can be used to determine exactly the right spot to inject the hyaluronic acid. In general, the procedure is painless, and patients notice relief from symptoms after some days. In knee joint injections, patients walk out of the office without any assistance and should not stop daily activities. More than one injection per year can be performed, but we follow clinical and pharmacological criteria for determining the frequency and periodicity of the procedure.
What are the most frequent cases in your practice?
Chondromalacia patella (cartilage wear and tear) in women is becoming increasingly more frequent. They experience a lot of pain going up and down stairs and a grinding sensation on the knee area, they may have a lot of difficulty squatting and going down hills. They often describe what we call the cinema sign: a lot of pressure on the anterior region of the knee during prolonged periods of sitting (such as in a movie theater). This condition can severely impact a woman’s life and cause important limitations in daily activities. With a careful evaluation and correct clinical assessment, viscosupplementation can be very successful.
Another frequent condition is osteoarthritis. Even when the degenerative process of the joint is in its early and moderate stages, patients may already experience a lot of pain and, with the procedure, we can greatly improve their quality of life. Medication also helps maintain joint health in the medium and long term and can often prevent arthroplasties and other future surgical procedures. I emphasize that any medical procedure must be carried out under strict medical criteria and a prior evaluation is indispensable for the success of the treatment. We are always available to help determine the best treatments for each patient on a case-by-case basis.
Arthroplasty is the replacement of the damaged joint with artificial implants. These implants (protheses) are used when there is a very large joint wear. The main symptom in these cases is pain. Combined with other symptoms, patients’ quality of life is greatly affected. Often those close to the patients do not notice the condition at first because it is a slow and progressive disease. Patients may experience one or several of the following: loss of mobility and independence; need for a cane, crutches, wheelchair and/or caregivers to help with simple day-to-day tasks; depression; confinement at home; social exclusion; loss of mental faculties and worsening of senile dementia. Replacing the joint — be it hip, knee or any other — is a big responsibility. Replacement surgeries are major procedures and there are several possible complications. Therefore, they require preoperative preparation and very meticulous postoperative care. An experienced surgeon with a highly specialized team is indispensable, as are empathetic doctor-patient relationship and assertive communication. Explaining all the details of the procedure, home adaptations and recovery phases are part of the process and not always done so carefully.
How is the patient’s recovery?
We work in the best way and with the best medicine has to offer in order to promote the earliest possible recovery. Our rehabilitation protocol starts either on the same day of the surgery, or on the next day depending on the scheduled time of the procedure. Physical therapy techniques are used to stimulate the new joint and our clinical staff evaluates and monitors blood and other laboratory values. Hospital staff are thoroughly instructed, and we stay in direct contact to follow daily evolution. Hospital discharge takes place very safely and quickly. This way, we avoid infections and secondary complications and return patients to their homes and families as soon as possible. Outcome is spectacular. With a highly specialized and committed team, we greatly reduce the possibility of any adverse event and patients experience substantial improvement in quality of life.
How can I get you to perform an arthroplasty on me?
I usually say that complex procedures are like a marriage. We start with an in-office evaluation. If surgery is recommended, we start a process that goes through medical history and physical evaluations and a very careful preoperative preparation with several exams, comorbidity evaluation, medication reconciliation and a detailed checkup. Depending on the case and complexity, our anesthesia team performs a pre-anesthesia evaluation for scheduling and planning. We will have two or three appointments before surgery. I will guide you through every step, answering questions and aligning all aspects of home planning and patient care. When we are completely confident and patients are fully prepared for surgery, we perform the procedure. I only work with high-quality imported prostheses. We visit patients daily during the entire length of their hospital stay.
Schedule an appointment and see if this marriage is the right one for you.
What type of prosthesis do you use?
Always the best ones available in Brazil. I really like American implants, but in some cases I can use German or French ones. The choice of technique and material depends a lot on the patient, and it is only possible to confirm after a previous medical evaluation. We will always choose the type of prosthesis that best meets our patients’ needs.
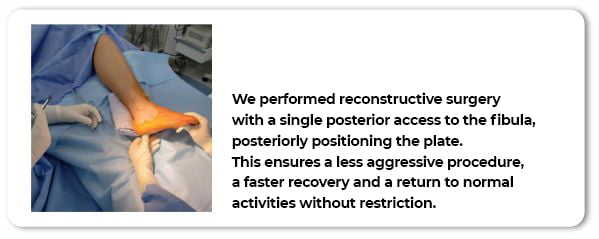
It is impressive how athletic performance has been improving. Consequently, injuries have also been increasing exponentially: repetitive and highly intense physical activities can cause too much stress to the body, which ends up causing a higher incidence of orthopedic injuries. These injuries often happen at the same time, affecting different tissues of the same joint (e.g.: knee ligament and meniscus, tendon and insertion bone, meniscus and cartilage, among others). In these cases, attention to the details of the injury, the patient’s individuality, and the sport practiced are fundamental aspects for choosing the best procedure and physical rehabilitation. What sets us apart is that we have specialized physical therapists for each area of the body who take care of the preoperative physical preparation (gain of range of motion, reduction of edema and inflammation, improvement of muscle activation pattern, improvement of blood circulation) and use specific techniques in the postoperative period to accelerate patient rehabilitation. We do not only aim to treat the injury, we aim to return the patient to sport with muscle quality and near preinjury performance. In the final stages we focus on proprioceptive exercises and joint protection, this helps improve balance while also reducing the risk of injury.
What is your experience with athletes?
As an orthopedist, I had the privilege of coordinating the medical department of the Deborah Colker dance company. Ballet dancers are true athletes, the intensity of the activity is enormous, therefore injuries are frequent. The time I spent at the company was very interesting, because I understood the importance of knowing the sport — its gestures and biomechanics — and also the athlete’s profile in order to make the correct recommendation for surgery and rehabilitation. I also learned how essential it is to work in a direct and positive manner with other professionals to promote a safe and quick return to work. Athletes need to practice to perfect their performances in sport. Staying inactive due to a long recovery period has a huge impact on their careers and can mean early retirement or moving to the “B team”. Last, but not least, I learned that there is a correct time for each step. Moving too fast through recovery stages can jeopardize the entire treatment.
Another interesting experience I had was with MMA and fighting athletes. I operated on athletes injured at an event in New York, provided second opinions and treated UFC athletes, and operated on One Championship and Bellator athletes. These athletes are incredible. They learn to fight with excellence in different fighting styles. Physical performance should always be as high as possible in this contact sport. I achieved substantial results working on these athletes — a source of great pride — due both to prior experience in surgeries and rehabilitation of athletes and a robust team of multidisciplinary specialists by my side. Once again, knowing kinetics/kinematics, biomechanics, studying the sport’s gestures and working with excellence in surgery and rehabilitation are the key to success. Few medical teams have this complex apparatus.
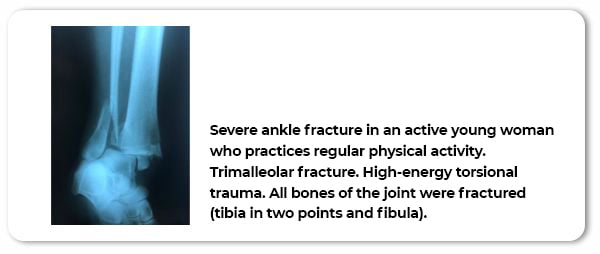
We call it a fracture when a bone “breaks”, loses its ability to withstand load and stops supporting tissues and muscle mass. When the fracture affects the joints, they are considered even more serious. This is because it is in the joint where movement occurs, enabling walking, picking up objects and interacting with the environment. Badly managed injuries can cause major functional repercussions and even permanent sequelae with adverse consequences in professional and personal lives of patients.
Fractures in elderly patients deserve special attention. These are more fragile individuals, with slower metabolism and weaker bone structure. Most of the time, they suffer from other previous conditions and tend to take more prescription medication than younger patients. The team that works with these patients needs to be very well-adjusted and experienced to better understand the medical aspects and physiology. Anesthetic strategy must be sound and a fast, effective, and minimally invasive surgical technique is the best option. The postoperative period must be conducted with great expertise and physical rehabilitation must be very well guided in order to achieve the best results.
I work with a multidisciplinary team that provides state-of-the-art high-quality care in all stages of the process: a mindful and attentive preoperative care personnel, an anesthesia team with expertise in orthopedic patients, surgeries with the most modern implants on the market and perfect bone reconstruction. We guide and monitor all stages of rehabilitation to achieve the best outcomes.
If a relative of mine is admitted to a hospital, can you evaluate and treat them?
Yes. This is a fundamental part of the process. I go personally or send my team to the hospital where the patient is admitted. We evaluate the overall medical condition. We interact with the hospital staff and work alongside them. We read the medical records and evaluate the images, determining the severity of the condition and the best treatment option. We are fast and respond immediately. We are punctual, compassionate and we will always do what’s best for our patients. We can go to any hospital in Rio de Janeiro or Niterói whenever someone is in pain and in need of our care. You need only contact us.
But the hospital already has an orthopedic team. I don’t know who the doctors are, and I have no reference. I would like you to perform the surgery, is that a problem?
Absolutely not. The decision of who will operate or manage an inpatient is always up to the patient and their family. We have worked in several different hospitals in Rio and Niterói and got to know most of the teams in the most important ones. We always act with great cordiality and use the resources of each hospital to best serve our patients. Once we take over the case, we manage everything quickly and with excellence.
Trauma is one of the noblest specialties in orthopedics and is often conducted by professionals who are not specialists in the area. Orthopedic trauma deals with any severe injury to the bones, joints, and/or soft tissue that is caused by an external source. Trauma (and polytrauma) also causes major repercussions on several other organs and tissues. Management of these cases by unqualified professionals can lead to serious complications: prolonged time in intensive care, prolonged hospital stays, secondary infections and even death. These unfortunate outcomes are not uncommon. Car accidents, falls from great heights, and even falls at home (generally in elderly patients), bring a great challenge to the medical professionals involved. They need to have great expertise to determine the ideal time for the approach and choose the best surgical technique. A multidisciplinary team capable of maintaining the patient in the best clinical condition is also essential.
I didn’t understand why orthopedic trauma patients are so serious and need so much care. Can you explain it to me?
Trauma evokes an inflammatory process that accelerates the metabolism and consumes a lot of energy. Patients arrive at the hospital very weak. In addition, they did not undergo surgical preparation, whether clinical or psychological. Trauma is an acute, sudden, and unexpected event. Therefore, we have to be fast to prepare the patient quickly and, believe me, every minute makes a difference, and a highly trained team is of great importance at this moment. Knowing how to approach the family, being present, welcoming the patient is also an indispensable aspect. The trauma surgeon must know how to operate using different techniques to determine the one best suited to the patient. A bad choice can further weaken the patient leading to a negative outcome. I am a specialist in orthopedic trauma surgery, a full member of the Brazilian Society of Orthopedic Trauma with national and international experience having coordinated the most important trauma emergency services in Rio de Janeiro (INTO, Hospital Copa D’or and Hospital São Lucas de Copacabana — CURRENT COORDINATOR). My master’s thesis in 2016 was an in-depth study evaluating the most important aspects of hip fractures (hip breakage in an accident) and was later published in the Brazilian Journal of Orthopedics (RBO). I reviewed all the techniques and their outcomes and established criteria that help the surgeon choose when to operate and the best surgical approach. Our team has clinicians specialized in the preparation and follow-up of patients with this profile and experienced anesthesiologists who always work in pairs (many services and teams work with only one). The physical therapists have been working together for years and are already in tune providing fully coordinated care. We work in a meticulously built team of high-level professionals. I don’t accept anything less than the best for my patients and that’s why the results are very substantial.
What are the main fractures and causes that you observe in your daily practice?
It is very interesting that it can vary even depending on the climate and temperature. On sunny days, we see many ankle and wrist fractures from accidents during soccer matches. Accidents on bike lanes and beaches also increase. On colder days and in neighborhoods with a higher concentration of elderly people, femur fractures are the champions. Generally, elderly people fall at home and get seriously injured, requiring hospitalization for osteosynthesis (fracture fixation) or arthroplasty (replacement with a prosthesis).
A relative of mine was admitted to a hospital, can you and your team take over and manage their case?
Of course. The decision of who will take care of their loved one is always up to the family and to the patient. In cases that require a more complex care, we can even transfer them to a high complexity center. A fully equipped ambulance picks them up and we use the most modern resources for comprehensive care. We work in all hospitals in Rio and Niterói. Our team is agile and multidisciplinary. I have a complete and highly specialized team in the treatment of hospitalized and critical patients.
How do I get you to take over the case?
It’s very simple. Give us a call on the number provided above. We will talk and evaluate the case. Once the family opts for our specialized treatment, we immediately go to the hospital and take all necessary measures to ensure the best treatment for the patient.
Dr. Daniel Ramallo dreamed of becoming a doctor since childhood. A dream that required dedication, abdication, and effort. He devoted himself to his studies to best serve his patients with state-of-the-art care in a highly personal, comprehensive and compassionate manner.